Many cancer care teams treat patients with a combination of therapies, sometimes called polytherapy. These treatments may be prescribed one after another, or sometimes, concurrently, meaning at the same time. In some cancers, the dual treatments can make a great difference in eliminating a tumor, controlling growth of a tumor, and preventing or controlling cancer that has spread to another part of the body.
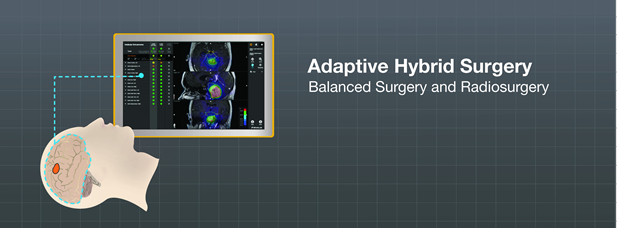
Adaptive Hybrid Surgery
Benign brain tumors are non-cancerous or non-malignant. They typically grow slowly, do not invade surrounding tissue, do not spread to other organs or tissue and are usually discovered by CT or MRI brain scans. These non-malignant tumors need to be removed once they begin to impact critical brain function due to growth. Because these tumors are non-cancerous, surgeons do not want to take any risks when removing them, so that patients leave the hospital in the same mental and physical state as when they entered.
If a patient has been diagnosed with a small benign brain tumor that is not causing any issues (asymptomatic), the cancer care team will likely prescribe stereotactic radiosurgery as a stand-alone treatment.
A growing number of patients with benign brain tumors, especially skull base tumors, now undergo partial surgical removal of their tumors. This is called ‘subtotal resection, and it means that most, but not all, of the tumor is removed. Some of the tumor is left behind on purpose because removing that last part poses a high risk for damage to critical brain structures. This treatment practice lowers the risk of brain damage to patients and is considered ‘standard of care’ for many brain tumor procedures.
An adaptive hybrid approach is a balancing act between removing more tumor—putting the patient at greater risk for surgical complications—and resecting less, which requires the patient undergo more potentially toxic radiation.1 95% of all treatment-related toxicities—including mortality—happen during the removal of the last 5% of the tumor in subtotal resection of benign brain tumors.2
The drawbacks to ‘subtotal resection’ are that patients move into a ‘wait and see’ pattern, post-surgery, so that their doctors can monitor any tumor regrowth. This continued follow-up is very important, but may cause anxiety for patients looking for finality with their cancer and treatment regimen.
The statistics associated with ‘subtotal resection’ are only slightly better when compared to ‘total resection,’ given the need to re-operate due to tumor recurrence.2
When any tumor regrows, the patient must again undergo treatment, which typically would be either another surgery or radiation treatment. Further surgery to remove the new growth poses risks, given the need to remove the entire tumor to prevent further regrowth. The ‘total resection’ poses the same potential for functional damage to surrounding brain tissues and structures as the original surgery.
Depending upon the size and volume of the tumor regrowth, radiation therapy may pose complications as well. These complications could have been avoided if the radiation had been given as follow-up to the original surgery, when most of the tumor was removed and the radiation was necessary for only a small volume.
The programmed addition of pre-planned stereotactic radiosurgery immediately after partial tumor removal is becoming increasingly popular for brain cancer treatment. New stereotactic radiosurgery (SRS) tools are now available, during surgery, to guide neurosurgeons. Sophisticated software provides surgeons with assistance in establishing the perfect crossing point between surgery and radiosurgery. The planned radiosurgery can be carried out as soon as a week after surgery but up to two months later. This timeline depends upon the doctors, hospital and even countries where Adaptive Hybrid Surgery is practiced.
Adaptive Hybrid Surgery helps to provide the optimal balance between both treatments – surgery and radiosurgery. [3] To learn more about Adaptive Hybrid Surgery, listen to Orin Bloch, M.D. on the Brainlab YouTube Channel at https://youtu.be/nzhx_LJI5eo.
Chemoradiotherapy
Combination treatments like chemoradiotherapy (CRT) are becoming more popular, especially in the treatment of some head and neck cancers as well as brain tumors like glioblastomas and sarcomas. Combining certain chemotherapy drugs are thought to help sensitize the radiation, making it more effective because it creates a systemic effect on top of the local effect of the radiation. The idea is that giving smaller doses of both therapies at the same time may achieve the same results as giving higher doses of each separately. These lower doses may also reduce radiation toxicity and also lower or eliminate the necessity of surgery.
While there are many benefits to this type of treatment for certain indications, it is wise to discuss thoroughly the potential side effects of an intense combination regimen using chemotherapy and radiotherapy.
Intraoperative Radiation Therapy
Intraoperative Radiation Therapy (IORT) is another combination therapy where radiation is delivered during surgery to remove a tumor. The radiation is given as a single dose to the area where the tumor has been removed. IORT may help to kill any microscopic disease tissue that still remains, reduce radiation treatment times in follow-up therapy, and add a radiation ‘boost’ to the cancer treatment.
While IORT has been available for many years, it is still considered relatively experimental for most cancers, although its benefits are being evaluated for certain indications. This treatment is not widespread, partly due to complicated delivery methods, sterility challenges and extended surgery time required.
Patients must be surgical candidates before IORT is considered. Doctors will thoroughly analyze the patient’s individual diagnosis, tumor type and personal preferences before recommending a course of treatment.
1 http://www.braintumorinstitute.org/pdfs/June2014_breakthroughs.pdf
2 https://youtu.be/nzhx_LJI5eo [7:53]
3 I.J. Barani, A.T. Parsa.Adaptive Hybrid Surgery: Feasibility of Planned Subtotal Resection of Benign Skull Base Tumors Followed by Radiosurgery to Minimize Morbidity Without Compromising Tumor Control. Int. Journal Rad. Onc., November 1, 2012. Volume 84, Issue 3, Supplement, Pages S278-S279.