Doctors use radiation to target cancer cells with the goal of stopping brain tumor growth and destroying the cells. The radiation works by damaging the DNA of the cancerous cells, which causes those cells, or targets, to shrink and die. Radiation can also affect nearby healthy cells, but they usually recover at a faster rate than the cancer cells. However, doctors try to prevent potential side effects that can happen when healthy tissue is exposed to the radiation by protecting them with different methods. The methods can include low dose radiation, treatment sessions that are spread out over time, newer techniques that allow for more precision-focused treatment, and drug therapies can help protect parts of the body from the radiation.
Your medical team will assess your specific brain tumor and its sensitivity to radiation based on several different factors, which may include the type of cancer, size and number of tumors and placement of tumor(s). Depending upon the type of radiation therapy your doctor prescribes, the way that the cancer-fighting treatment is delivered will differ.
Go to What is Radiation Therapy for more information on external beam radiation therapy including stereotactic radiosurgery and fractionated stereotactic radiotherapy.
You will work with your cancer team to discuss all the options and decide upon the best course of treatment based on your cancer.
Hardware
Radiation is typically delivered using a machine called a linear accelerator or a cobalt-60 system.
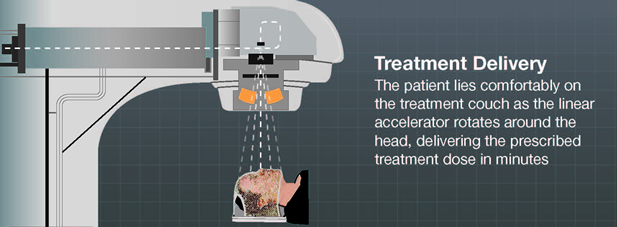
When a linear accelerator is used, the treatment X-ray, or beam, comes from the machine’s head, called the gantry, and can be circular or shaped to the tumor. While the patient lies on a specially designed treatment couch, the linear accelerator rotates around the patient’s head, delivering the radiation beams to the tumor from different directions and angles. By doing this, the tumor receives the most radiation while the healthy tissue around the tumor receives less radiation.
Advancements in LINAC hardware include mechanics that allow doctors to shape the radiation very precisely1,2 to the shape of the tumor. This helps reduce the radiation to healthy tissue while at the same time allows a higher dose of cancer-fighting treatment to be delivered to the tumor. This option also offers a ‘frameless’ or non-invasive treatment option.
Another option is stereotactic radiosurgery using a cobalt-60 system. This system delivers the radiation beams through about 200 pinholes, which meet or converge, at the tumor site, allowing a high dose of radiation to be delivered to the cancer, while sparing the surrounding tissue. The patient is secured with a head frame when this device is used, so there is no movement during the procedure and accuracy can be assured.
There are many different treatment options on the market. It is best to discuss your specific brain tumor with your cancer care team and which type of treatment may work best for your condition.
Treatment Planning Software
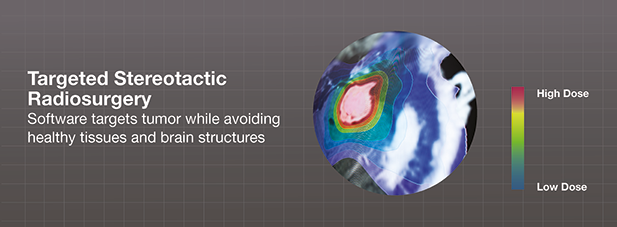
Ever-evolving technology advancements allow doctors to better plan, or simulate, the radiation therapy before delivering it by using detailed imaging scans. The software allows the cancer team to plan the therapy and accurately3,4 deliver the treatment dose to the tumor while at the same time protect the healthy tissue and brain structures around the tumor as much as they can.
Stereotactic radiosurgery, considered standard of care for small benign brain tumors, allows doctors to achieve a ‘surgery-like’ result without the complications that can arise with traditional surgery. It also offers hope for patients with tumors that have been deemed inoperable. The strong radiation dose required by this type of treatment requires high accuracy, solid patient fixation, sophisticated patient positioning and precise dose calculations.
Specialized and dedicated radiosurgery software offers many benefits to the cancer treatment team and therefore to their patients. Clinicians can verify and validate important functions like avoiding radiation to important structures such as the brain stem or facial nerve.
Planning software can take into account the importance of adequately mapping out the treatment with precise tumor outlines and proper ‘dose gradients,’ so your doctor can analyze how the radiation decreases from a high point at the tumor’s center to lower at the tumor’s edge to almost nothing for nearby surrounding healthy tissue and brain structures.
The newest and most advanced software tools utilize techniques amassed from leading medical experts in the field of stereotactic radiosurgery. The tools offer automation and consistency, which help doctors customize the treatment plan to each patient and his or her tumor.
Doctors can use sophisticated software to plan the desired treatment to the tumor while avoiding healthy tissues and critical brain structures.
Image Guided Radiotherapy
There are many different techniques used to deliver radiation to tumors. In the positioning of the patient prior to and during treatment, images are used for accuracy and to detect any movement. When the images are generated in the radiation treatment room, the process is called image guided radiotherapy (IGRT).
Progress across all the different specialty areas has grown to include advanced computer simulation and image guidance technologies that are used both before and during radiation therapy. These sophisticated computerized systems are used throughout the patient setup and treatment delivery to help position the patient correctly and in line with the three-dimensional diagnostic images.
Radiation therapy software, at the highest level, can offer doctors detailed information about the shape, size and position of a tumor, guide setup and patient positioning and monitor tumor motion during treatment.
1 van Santvoort et al., IJROBP 72(1), 261, 2008
2 Lamba et al., IJROBP 74(3), 913, 2009
3 Ramakrishna et al., Radiother Oncol 95, 109, 2010
4 Feygelman et al., J Appl Clin Med Phys 9(4), 68, 2008