Radiation therapy (RT) is also called radiotherapy and is a common type of treatment for brain cancer. Radiotherapy uses the same kind of radiation as is used in radiology, which is a more familiar term. Radiotherapy uses X-rays and other high-energy radiation to treat cancers whereas radiology uses lower doses of the same radiation types for imaging and in the diagnosis of disease.
There are different types of radiation therapy and different technologies used in radiation therapy. For the discussion of brain tumors, we will focus on the types and technologies of radiation therapy that are most common and beneficial in treatment of these types of conditions.
Radiation therapy uses high doses of radiation—such as those from X-rays, gamma rays, or other particles—to stop or slow the growth of a brain tumor. This is different from low dose radiation, which is used in radiology for imaging (X-rays, MRI, CT) broken bones or teeth. The cancer-fighting, high-dose radiation treatments can be delivered in different ways, the most common of which is called ‘external beam’ radiation therapy and is given from outside the patient’s body. More than half of people with cancer (about 60 percent) get radiation therapy as a treatment option.1
There are different treatment types when considering radiotherapy for brain tumors. Stereotactic radiosurgery (SRS) is a radiation therapy procedure that uses special equipment to position the patient with sub millimeter precision2 and deliver a large radiation dose to a tumor and not to normal tissue.
Image guided radiotherapy (IGRT) offers advancements in treatment precision by incorporating computer imaging into the planning and delivery of the radiation therapy.
RT, SRS and IGRT are common brain cancer treatments prescribed by radiation oncologists – doctors who specialize in giving radiation therapy treatments. In most hospitals, a team of cancer specialists including the radiation oncologist, surgeon, physicist, radiation therapist and nurse work together to develop a personalized treatment plan for each patient. Radiation therapy can be used alone or as part of a broader treatment program, which could also include other treatments like surgery or chemotherapy.
External beam radiation therapy can be given in a single treatment or over several appointments, called fractions, or sessions. The sessions can be once a day, five days a week and can last between two and ten weeks, depending upon the type of brain tumor and the goal of the treatment.
Your cancer care team may prescribe your radiation with different schedules, depending upon your diagnosis and overall treatment plan. You may receive your total radiation dose over a shorter number of days than traditional radiation therapy or in unique situations, you may receive small doses of radiation more than once per day.
There continues to be great advancements in the field of radiation therapy. If you and your doctor decide that a form of radiation therapy is the right next step for you, you may be interested in learning more about the different options available to your cancer team. Explore more about the different treatment options in the Radiotherapy versus Radiosurgery section.
Whole Brain Radiation Therapy
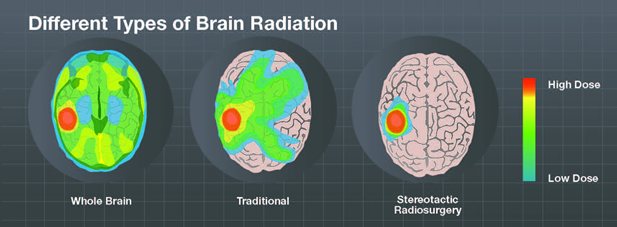
Whole brain radiotherapy (WBRT) delivers the radiation dose to the entire brain. It is often used to treat cancers that have spread to the brain, called metastases, although this procedure is becoming less common as advancements are made in other radiation treatment options.
Patients with limited brain metastases suitable for stereotactic radiosurgery (SRS) should be treated upfront with organ sparing SRS, and no longer with whole brain radiation therapy (WBRT).3
Stereotactic Radiosurgery for Brain Tumors
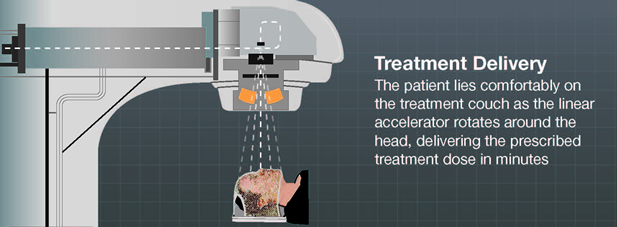
Stereotactic radiosurgery, sometimes called ‘knifeless’ surgery, is a form of radiation that was originally developed specifically to target brain tumors. The patient receives a single high dose of radiation using technology that precisely aims and shapes the radiation beams, from many angles, onto the targeted tumor or lesion as the system rotates around the patient’s head.
The origin of the word ‘radiosurgery’ comes from the way the treatment is typically delivered – targeted high-energy radiation delivered in a one-time session. This does not mean any incisions are made like in a typical surgery, just that the treatment is only delivered once, compared to other forms of radiotherapy, which are delivered over the course of many sessions, also called fractions. Stereotactic radiosurgery is different from whole brain radiotherapy (WBRT) treatments, where the patient receives radiation that blankets the whole brain.
Stereotactic radiosurgery offers sophisticated software and delivery systems, which allow doctors to focus radiation precisely at the brain tumor, while simultaneously protecting surrounding healthy tissue and brain structures.
Advanced, high definition treatment machines can shape the beam very precisely to the brain tumor and then move around the patient’s head to deliver the treatment from different angles so that the healthy tissue receives less radiation but the brain tumor receives a concentrated dose throughout the treatment. Stereotactic radiosurgery is becoming more common for many types of brain tumors and is especially effective for tumors that are hard to reach or have been considered ‘inoperable’ in the past.
Radiosurgery has become the preferred treatment for a significant portion of benign brain tumors with very high tumor control rates and similar rates of trigeminal, acoustic, facial and cranial nerve preservation compared to surgery.4,5
Some SRS systems now also offer non-invasive, or ‘frameless,’ treatment options for patients. Traditionally, the patient must wear a stereotactic headframe before and during the treatment to help with positioning and treatment accuracy. The frameless option now allows patients to be fitted with a personalized mask that helps keep them still during treatment but is not fixed to the head. State-of-the-art image guidance technologies allow for precision positioning and monitoring of the patient throughout the treatment helping ensure desired outcomes.6
Most recently, stereotactic radiosurgery has been expanded to also include treatment that includes up to five different sessions, which is called ‘fractionated stereotactic radiotherapy.’
When compared with frame-based stereotactic radiosurgery, frameless SRS can provide non-invasive treatments at equivalent accuracy, faster treatment delivery, more flexible treatment scheduling and a higher level of patient comfort.6,7,8
1 National Cancer Institute ‘Cancer and You’ http://www.cancer.gov/publications/patient-education/radiationttherapy.pdf
2 Murphy E. S. et al., Int. J. Radiat. Oncol. Biol. Phys. 79, 985–97, 2011
3 Sahgal, A., Larson, D. & Knisely, J. Stereotactic radiosurgery alone for brain metastases. Lancet Oncol. 16, 249–250 (2015).
4 Badakhshi H. et al., J. Radiat. Res. 1–5, 2013. doi:10.1093/jrr/rrt101
5 Murphy E. S. et al., Int. J. Radiat. Oncol. Biol. Phys. 79, 985–97, 2011
6 Verbakel W. et al., Radiother Oncol 97, 390, 2010
7 Gevaert, T. et al. Setup Accuracy of the Novalis ExacTrac 6DOF System for Frameless Radiosurgery. Int. J. Radiat. Oncol. Biol. Phys. 82, 6 (2011)
8 Rad Fan, 2011 April (Vol.9 No.4)